Abstract
Metabolic reprogramming is one of the hallmarks of cancer, as these rapidly dividing cells need to adapt their metabolism to cope with an increased energy demand. We have previously showed that in mouse models of myeloproliferative neoplasms (MPN), JAK2-mutant cells display metabolic alterations, including increased oxidative phosphorylation and glycolysis. The glutamine-glutamate-alphaKetoglutarate (aKG) axis, besides fueling the Krebs cycle and anabolic processes, contributes to the synthesis of the heme precursor 5-aminolevulinic acid (5-ALA), thus making glutaminolysis a potential target for MPN therapy.
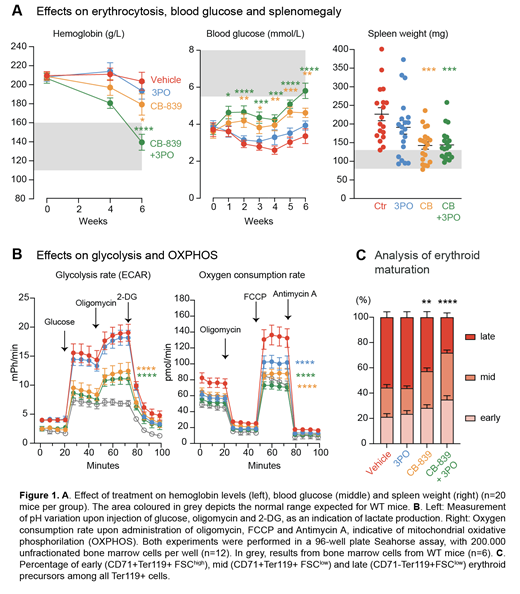
Here, we examined the effects of pharmacological inhibition of the conversion of glutamine to glutamate by glutaminase 1 by Telaglenastat (CB-839) in a mouse model of JAK2-V617F driven MPN. We performed competitive transplantations of bone marrow co-expressing JAK2-V617F with a GFP-reporter and wildtype mice in a 1:10 mixture into lethally irradiated mice. At 8 weeks post-transplantation, the mice developed MPN phenotype and were randomized into 4 treatment arms. They were then treated for 6 weeks with vehicle, CB-839, 3PO (6-phosphofructo-2-kinase inhibitor) and the combination of CB-839 + 3PO. We found that hemoglobin levels were significantly reduced in CB-839 treated mice and were fully normalised in mice that received a combination of CB-839 + 3PO (Fig. 1A). Other peripheral blood cell counts did not change (not shown). Hypoglycemia was noted in the vehicle group, as previously described, but an increase in blood glucose levels was seen already after one week of treatment with CB-839. 3PO alone had less impact on hypoglycemia and mice receiving CB-839 + 3PO had similar values to CB-839 alone (Fig. 1A). In line with these findings, splenomegaly was also reduced (Fig. 1A).
To characterise the changes in metabolic activity, we determined the metabolic profiles of unfractionated bone marrow (BM) cells using seahorse assays. As expected, basal and maximal glycolysis and oxidative phosphorylation were higher in vehicle treated MPN cells than cells from wildtype controls. However, when BM cells from CB-839 or CB-839 + 3PO groups were examined, they displayed a strong downmodulation of both glycolysis and oxidative phosphorylation, indicating that chronic exposure to CB-839 reprograms the metabolic machinery by reducing not only the basal glycolytic and respiratory levels, but also the maximal capacity (Fig. 1B).
Glutamine is the primary source of aKG needed to produce the heme precursor 5-ALA, and hemoglobin synthesis consumes the majority of ATP in erythroid progenitors. We therefore hypothesize that 5-ALA shortage caused by CB-839 limits hemoglobin production, leading to reduced catabolic activity and drop in ATP demand. To evaluate this model, we examined the stages of erythroid differentiation from vehicle or treated mice. Early and intermediate erythroid cells were enriched at the expense of later stages in CB-839 and CB-839+3PO treatment arms (Fig. 1C). The accumulation of erythroid precursors at the stage before hemoglobin is assembled supports the hypothesis that targeting glutamine usage impairs excessive erythropoiesis by limiting hemoglobinization rate.
Our data show that inhibiting glutaminolysis ameliorated MPN phenotype and that the combination with the glycolytic inhibitor 3PO was able to induce complete hematological response. Since CB-839 is already in clinical trials for other cancers, our data suggest that it could also be tested for treatment of patients with polycythemia vera.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal